1. INTRODUCTION
Orientia tsutsugamushi (OT), a causative agent of acute febrile disease scrub typhus, belongs to the Rickettsiaceae family in Rickettsiales. The term “scrub” is used due to the vegetation type that bears vector. The word “typhus” is derived from the Greek word “typhus,” which means “fever with stupor or smoke” [1], “Tsutsuga” means “small and dangerous,” and “Mushi” means “insect or mite.” It requires a host cell for growth as it is an intracellular bacterium. According to the World Health Organization, it has been categorized as one of the world’s most underdiagnosed/underreported diseases [2]. Electron microscopy has revealed that the structure of the outer envelope, the outer membrane cell wall is thicker than the inner membrane. At the same time, it is totally reversed in other species of Rickettsia [3]. The difference in 16s rRNA sequence and some morphological and biochemical characteristics is the main reason that the bacterium has been recently transferred to genus Orientia, which is newly added in the Rickettsiaceae family [4].
Leptotrombidium mites transmit OT during their larval stage of development, known as “chiggers.” The incubation period is 6–21 days. Clinically, it can be distinguished by high fever, rash, eschar, lymphadenopathy, pneumonitis, and meningitis. If untreated, it can lead to severe multiple organ failure and death [5]. The mortality rate range from 1 to 40%, depending on different endemic areas and encountered strains of OT [3].
2. METHODS
2.1. Data Sources
Epidemic-prone diseases are collected from the Integrated Disease Surveillance Program (IDSP) weekly which comes under the national center of disease control. Most of the data were collected from scientific databases such as PMC-NCBI, Google Scholar, PubMed, Scopus, and Scientific index. A systematic literature review of epidemiological studies of scrub typhus was carried out in this analysis from the epidemiological exposure records.
2.2. Study Eligibility Criteria
The main collection criteria are based on clinical manifestation with the presence of eschar and laboratory diagnoses such as enzyme-linked immunosorbent assay (ELISA), Weil-Felix (WF) test, IFA test, or nested polymerase chain reaction (PCR) test targeting a 56-kDa gene clinical presentation symptoms and specific complications. Figure 1 illustrates the Preferred Reporting items for Systematic Review and Meta-analysis (PRISMA) flow diagram of identification, screening, eligibility, and inclusion which include in our search criteria. Approximately 324 reports have been collected from different sources and many of them were excluded as those have no clear evidence. In the end, 133 articles met the selection criteria and were approved for the analysis.
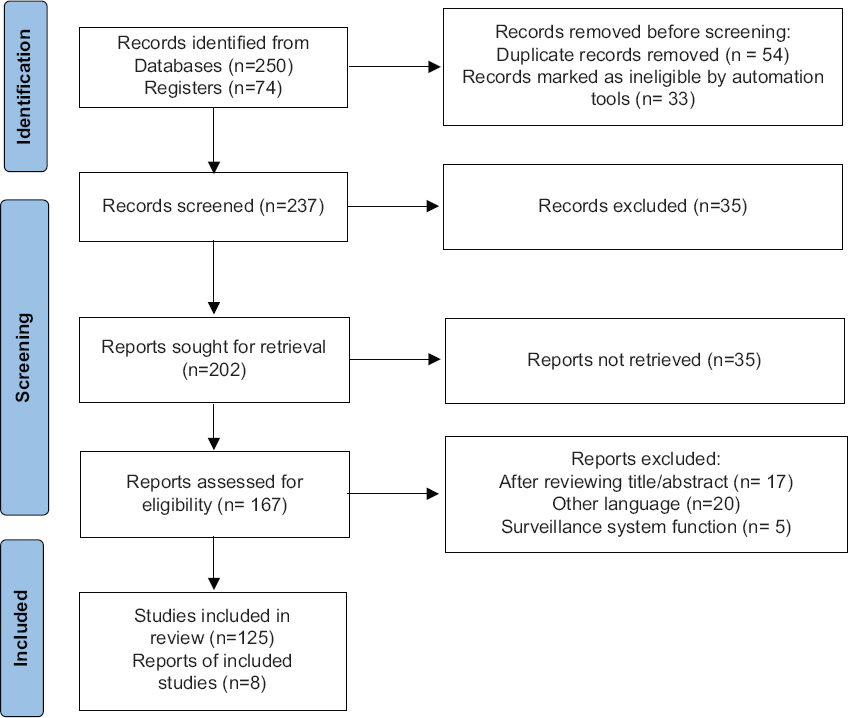 | Figure 1: The study selection process for the included, data are represented by the PRISMA flow diagram. [Click here to view] |
2.3. Statistical Analysis
Although this is a review article, no specific statistical analysis is done. The data are based on mean standard deviation, analysis by student t-test, Chi-square test, or Fisher exact test was considered as many researchers presented in their research articles. Mostly, P > 0.05 was supposed to be statistically significant.
3. RESULTS
3.1. Geographical Distribution and Global Outbreak
Although this disease has been recognized since 313A.D. and has threatened billions of people in different regions of Asia and Australasia, it is still considered an underdiagnosed and underreported illness [6]. Previously, it was restricted to a specific area ranging from Russia to Japan in the north, Northern Australia in the south to Pakistan, and Afghanistan in the west known as the “tsutsugamushi triangle” ranging a broad area of 13 million km2 [Figure 2] [7]. However, there are confirmed cases of increasing and spreading in other areas such as Dubai, United Arab Emirates [3] Chile, Peru, and Africa. During World War II, confederated forces suffered more destruction due to scrub typhus than the different outcomes of the war in Southeast Asia [8]. The diversity of species and epidemic characteristics in other countries such as China, Japan, South Korea, Taiwan, Hong Kong, and Thailand is represented, as a graph shown in Figure 3 [4-13].
 | Figure 2: Geographical distribution of scrub typhus in tsutsugamushi triangle. [Click here to view] |
 | Figure 3: Scrub typhus incidence in several endemic countries from 2000 to 2020. [Click here to view] |
The season of scrub typhus usually starts in May gradually increases every month; maximum cases were reported in June and July called pick months. The studies correlate with the climate and life patterns of organisms. From 2006 to 2016, there is a high rate of increased cases in China [9]. Compared to China, Japan showed the maximum cases during November [10]. Alike to Japan, October and November are the peak months in South Korea [11]. In South Korea, the Scrub typhus has been identified for the 1st time during the Korean War, but the disease was not revealed to the Korean population; however, until 1986, it was new to Korean citizens [12]. It has become widespread and regarded as the most widely recognized Rickettsia disease in South Korea. The age distribution differs in different countries. The age group varies in South Korea, that is, the patients of 60–69 years are supposed to be more affected [12]. The gender difference was not observed. In Japan, the most common age group was 51–75 years which was 62% of total reported cases, while in China, the suffered people of the same age group were <1/2 of the total patients [10]. In Thailand, the first human case was reported in 1952 [4] and the confirmed cases increased rapidly during 1980–2000, where 50–59-year-old patients were more affected [4]. In many of the cases, it has been seen that the main reason for the cause of scrub typhus disease and spread is the outdoor activity, working in farms and forestry, uneducated, and lifestyle. Furthermore, the articles showed that rural people are more supposed to be affected than people staying in urban areas.
Besides the countries narrated above, there are many other countries such as Taiwan, Hong Kong, Thailand, and the Maldives with scrub typhus reports in the tsutsugamushi triangle and southwest Pacific islands including Indonesia and the Philippines, and the landmass of Australia for almost a century [8,14].
3.2. Outbreak in India
Scrub typhus has an outbreak in different regions of India, but it spread out as an epidemic in Assam and West Bengal during the Second World War. The vector mites are primarily present in equatorial rain forests, subarctic terrains, and semi-deserts in the Himalayan regions as these are the diverse ecological niches. Heat and humidity give steady and supreme conditions to the transmission of the infection. These environmental niches are called mite islands or Typhus islands [15,16]. This disease mainly occurs during winter in southern regions, whereas in northern Himalayan states, it is seen throughout the rainy season. It has been seen that North India is prone to Scrub typhus disease. Outbreaks were seen in the sub-Himalayan belt; from Jammu to Nagaland, mainly found in the whole Himalaya region ranging from Kashmir to Assam, Eastern and the Western Ghats, and the Vindhyachal and Satpura ranges in the central part of India. Furthermore, in Maharashtra, Kerala, Karnataka, Tamilnadu, Uttarakhand, West Bengal, Himachal Pradesh, and Rajasthan, many cases of scrub typhus have been accounted [17] and considered as one of the most re-growing infections of the present time. Although it is widespread in India, still specific prevalence data are not available. In the past few decades, the Rickettsia disease and scrub typhus have shown exponential growth and expanded in India during the cooler months, especially from July to November [Table 1 and Figure 4] [18].
Table 1: Scrub typhus outbreak in India (By laboratory findings).
| Place | Year | Suspected cases | Diagnosis | Test | Symptoms | Death | References |
|---|---|---|---|---|---|---|---|
| Tamilnadu | October 2001–February 2002 | 27 | Doxycycline Chloramphenicol | Weil – Felix | Fever (<101°F) abnormal liver function abnormal renal function | 3 | [18] |
| Jammu | July–October 2002 | 12 | Tetracycline | Weil – Felix | Fever (<101°F) Malaise, eschar, cojuctival congestion | [29] | |
| Himachal Pradesh | 2004 | 21 | Doxycycline Azithromycin | Weil-Felix PCR | Fever, eschar, respiratory distress | 3 | [17] |
| Manipur | May–September 2007 | 38 | Doxycycline Azithromycin | Weil – Felix | Fever (<101°F), eschar, breathlessness, renal failure, headache, vomiting | 2 | [30] |
| Pondicherry | April 2006–April 2008 | 50 | Doxycycline | Weil-Felix Eschar | Fever (<101°F), Eschar, Multiple organ dysfunction, breathlessness | [22] | |
| Meghalaya | October 2009–January 2010 | 24 | Doxycycline Azithromycin Chloramohenicol | Weil-Felix ELISA IgM | Fever, splenomegaly, eschar, pain abdomen, altered sensorium, vomiting, lymphadenopathy, , hepatomegaly | [28] | |
| Tamilnadu | September 2010–June 2011 | 52 | Doxycycline | ELISA IgM Eschar | Fever, hepatomegaly, Splenomegaly, eschar, | [31] | |
| Himachal Pradesh | July 2010–December 2011 | 253 | Doxycycline Azithromycin | ELISA | High fever, Chills and rigor, myalgia, abdominal pain, lymphadenopathy, | 13 | [26] |
| Sikkim | January–December 2011 | 63 | Doxycycline Azithromycin | ELISA, RICA | Fever, eschar, hepatomegaly , polyarthralgia, vomiting | [32] | |
| Meghalaya | 2010–2012 | 96 | Doxycycline | PCR | Eschar, Fever, MODS | [27] | |
| Tamilnadu | 2010–2012 | 95 | Doxycycline | PCR | Eschar, Fever, MODS | [27] | |
| Himachal Pradesh | 2010–2012 | 72 | Doxycycline | PCR | Eschar, Fever, MODS | [27] | |
| Pondicherry | 2011–2012 | 68 | Doxycycline | Weil-Felix, ELISA, Eschar | Fever, Eschar, meningitis | [33] | |
| Andhra Pradesh | August 2011–December 2012 | 176 | Doxycycline | Weil-Felix | Fever, brethlessness, Renal failure, respiratory failure | 8 | [34] |
| Kerala | 2012 | 2 | Doxycycline | Weil-Felix | Fever, Myalgia, Headache, Vomiting | [35] | |
| Rajasthan | October–December 2012 | 42 | Doxycycline | ELISA IgM | MODS, renal impairment, ARDS, meningitis | 7 | [36] |
| Puducherry | September 2012–March 2013 | 28 | Doxycycline | Rapid immunochromato graphic, ELISA | Fever, myalgia, Headache, vomiting, nausea , malaise, lymphadenopathy (seen in children only) | [37] | |
| North East (Assam, Sikkim) | July 2013–December 2014 | 228 | Doxycycline | ELISA IgM | Fever, breathlessness, cough, jaundice, abdominal pain, renal failure, diarrhea, rashes | [38] | |
| Uttaranchal | July–November 2013 | 69 | Doxycycline | ELISA IgM | Fever, myalgia, , lymphadenopathy, hepatosplenomegaly, rash, headache | 1 | [39] |
| Andhra Pradesh | September 2013–December 2013 | 258 | Tetracycline | IgM, PCR | Fever, lymphadenopathy rashes, eschar | [40] | |
| Odisha | September 2014–February 2015 | 25 | Doxycycline | ELISA-IgM | Fever, eschar, Respiratory distress, splenomegaly, Abdominal pain | 1 | [19] |
| Uttar Pradesh | August–October 2016 | 46 | Doxycycline | ELISA | Fever Change in mental health | [41] | |
| North East (Assam, Nagaland, arunachal Pradesh) | 2014 December–2016 December | 278 | Doxycycline | ELISA- IgM | Fever, Acute encephalitis syndrome (AES) | [42] | |
| Odisha | April 2011–October 2013 | 50 | Doxycycline | IgM ELISA, Weil-Felix test | Fever, myalgia, Breathlessness, ARDS, liver and renal failure | [43] | |
| Odisha | 2014 | 25 | Doxycycline | IgM ELISA | Fever, shock, lymphadenopathy, hepatosplenomegaly, respiratory problem | [19] | |
| Odisha | June 2014–February 2015 | 40 | Doxycycline, Azithromycin | IgM ELISA | Fever, headache, cough, dyspnea | [19] | |
| Odisha | July 2015–December 2015 | 71 | Azithromycin | IgM ELISA | Fever, rash, myalgia, headache, lymphadenopathy, hepatomegaly | [21] | |
| Odisha | April 2015–October 2016 | 60 | Doxycycline | IgM ELISA | Fever, rash, myalgia, Abdominal pain, breathlessness, renal failure, pneumonia | [23] | |
| Odisha | January 2015–December 2016 | 101 | Doxycycline, Azithromycin | IgM ELISA | Fever, headache, lymphadenopathy, hepatosplenomegaly, respiratory distress, abdominal symptom | [24] | |
| Odisha | January 2016–January 2017 | 10 | Doxycycline | IgM ELISA | Fever, headache, myalgia | [44] | |
| Odisha | June–November 2017 | 201 | Doxycycline, Azithromycin | IgM ELISA | Fever, rash, myalgia, headache, lymphadenopathy, hepatosplenomegaly, | [45] | |
| Odisha | 2020 | 240 | Fever, rash, myalgia, headache, jaundice, acute kidney injury | IgM ELISA | Doxycycline | [20] |
 | Figure 4: The map of India showing the reported cases of scrub typhus by states during 2000–2020. [Click here to view] |
In IDSP, the epidemic-prone diseases are collected weekly under the national center for disease control. The cases reported to IDSP (https://idsp.nic.in/index4.php?lang=1&level=0&linkid=406&lid=3689) of scrub typhus from 2009 to 2020 are during the rainy season and cooler months which start mainly from June, and gradually, the reports are increasing till November and December. The pick month for scrub typhus is from August to September. Every year, the highest cases and deaths are from Rajasthan, Odisha, and Tamilnadu in different years, but the maximum cases and highest deaths are from the northeast region of India [Table 2 and Figure 5].
Table 2: Outbreak in India according to IDSP
| Year | Cases | Death | Month |
|---|---|---|---|
| 2020 | 143 | 8 | August and November |
| 2019 | 389 | 14 | August and November–December |
| 2018 | 628 | 8 | January and August–September |
| 2017 | 158 | 3 | June–August |
| 2016 | 427 | 6 | April–September |
| 2015 | 174 | 6 | August– November |
| 2014 | 202 | 1 | July–August and November |
| 2013 | 381 | 8 | July–September |
| 2012 | 276 | 8 | August–November |
| 2011 | 41 | 3 | September |
| 2010 | 4 | 1 | October |
 | Figure 5: Graphical representation of state-wise outbreak of scrub typhus. [Click here to view] |
3.3. Outbreak in Odisha
For a long time, scrub typhus was an unseen case in Odisha; for the 1st time in Odisha, 25 cases of scrub typhus were identified and admitted to the hospital in the pediatric department of Kalinga Institute of Medical Sciences, Bhubaneswar, during post-monsoon months of 2014 [19]. Still, this disease remains unnoticed and underreported in many parts of Odisha, and children end up with complications due to negligence. Most cases are collected from the capital city Bhubaneswar; other than that patients die due to lack of diagnosis and proper treatment [20]. The cases were from rural and forest areas as compared to urban areas. However, the pediatric scrub typhus is very common in Odisha and has an undifferentiated fever and varies with gender and activity. The data on scrub typhus in Odisha are still not sufficient for any conclusion. People should be more careful and concerned regarding their different lifestyle practices [21].
4. CLINICAL PRESENTATION AND DIAGNOSIS
Rickettsial infections were recorded from different parts of India [22]. People working outdoors suppose to be more affected than the people staying inside their homes or working in a close area [23]. The outbreak findings were done using serological diagnosis tests such as the WF test followed by ELISA (IgM and IgG), rapid immunochromatographic test, and molecular bases methods such as PCR-nested PCR. The most common serological test method, ELISA for antibody detection, is widely used for diagnosis due to its wide availability and cost-effectiveness. The IgM antibody was seen at the end of the 1st week at a significant level. IgG antibodies are seen by the end of the 2nd week [15]. In reinfection, IgG antibody appears by the end of the 6th day, but IgM levels are variable. Diagnosis of scrub typhus was confirmed when a patient with an acute febrile illness had positive serology for scrub typhus and also nested PCR positive, further strengthened by the presence of eschar [24].
5. COMPLICATIONS
The patients show the symptoms ranging from undifferentiated acute febrile illness of changing seriousness with manifestation such as fever, headache, cough, eschar, myalgia, lymphadenopathy to more dangerous multiple organ failure, and ARDS. High and continuous fever is the most common symptom in patients with temperatures of about 101°F or above for more than 1 week [21]. The incubation period varies from 6 to 21 days, mainly 10 to 12 days [25]. If the patients are left untreated, they develop serious manifestation in 2nd week such as pneumonitis, ARDS, myocarditis, renal impairment, and neurological involvement.
It has been seen that patients were well responded to the antibiotic therapy and not many cases of clinical drug resistance were found. Doxycycline and azithromycin were frequently used as compared to chloramphenicol and tetracycline [26]. The mortality rate of patients with scrub typhus depends on the circulatory load of OT and the type of strains [27]. Deaths are due to delayed identification, improper diagnosis, and drug resistance; such cases have been reported in different states presented in Table 1 [17-45].
6. CONCLUSION
Our study showed that OT infection was endemic to a specific area, but it is spreading worldwide and can cause outbreaks and deaths in the next few years if it remains the same. Higher variability among the strains makes the diagnosis difficult. Although doxycycline and azithromycin are effective antibiotics for the treatment of this disease, the diagnosis of scrub typhus is excruciating in India due to its varied clinical presentation, absence of eschar in many patients, and shortage of gold standard tests. Still, data from only these states are not sufficient to draw any valid conclusion about the seriousness of these agents.
7. FUTURE PROSPECTIVE
Till last decade, the disease was epidemic to specific areas. However, in this study, it has been seen that the disease is spreading throughout the globe, but still it is neglected and underreported. Our study will give insight to the researchers to monitor and implement strategies to improve the surveillance system. It will help to understand the severity and complications of scrub typhus and the need for a proper therapeutic drug for children. As well as, it will show the necessity of vaccine development. From a global survey, the genetic diversity can be studied further to identify the most virulent strain from different places which will be the key factor in vaccine development.
8. ACKNOWLEDGMENTS
We are grateful to Dr. G Sahoo, Dean, IMS & SUM Hospital and Dr. MR Nayak, the President, Siksha ‘O’ Anusandhan deemed to be University, Bhubaneswar, Department of Pediatrics, Institute of Medical Sciences & SUM Hospital, Bhubaneswar, Odisha, India also acknowledge Medical Research Lab for providing the laboratory facilities. Miss. Subhasmita Panda is a SOA research scholar (Regd. 2081611018).
9. AUTHORS CONTRIBUTION
All authors made a substantial contribution to the conception, design, and acquisition of data took part in drafting the article or revising it critically for important intellectual content. The authors agreed to submit the manuscript to the esteemed journal, gave the final version of the published, and decided to be accountable for all aspects of the work.
10. CONFLICTS OF INTEREST
The authors report no financial or any other conflicts of interest in this work.
11. ETHICAL APPROVALS
As it is a review article, ethical approval is not required.
12. FUNDING SOURCES
There is no funding to report.
13. DATA AVAILABILITY
All data generated and analyzed are included within this research article.
14. PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
1. Watt G, Parola P. Scrub typhus and tropical rickettsioses. Cur Opin in Inf Dis 2003;16:429-36. [CrossRef]
2. World Health Organization. WHO Recommended Surveillance Standards. Geneva:World Health Organization;1999.
3. Luce-Fedrow A, Lehman ML, Kelly DJ, Mullins K, Maina AN, Stewart RL, et al. A review of scrub typhus (Orientia tsutsugamushi and related organisms):Then, now, and tomorrow. Trop Med and Inf Dis 2018;3:8. [CrossRef]
4. Coleman R, Sangjun N, Frances S, Lerdthusnee K, Tanskul P, Monkanna T, et al. Occurrence of Orientia tsutsugamushi in small mammals from Thailand. Am J Trop Med Hyg 2003;69:519-24. [CrossRef]
5. Balcells M. Endemic scrub typhus-like illness, Chile. Emerg Inf Dis 2011;17:1659-63. [CrossRef]
6. Blacksell SD, Tanganuchitcharnchai A, Nawtaisong P, Kantipong P, Laongnualpanich A, Day NP, et al. Diagnostic accuracy of the InBios scrub typhus detect enzyme-linked immunoassay for the detection of IgM antibodies in Northern Thailand. Clin Vac Immu 2016;23:148. [CrossRef]
7. Kim G, Ha N, Min C, Kim H, Yen N, Lee K, et al. Diversification of Orientia tsutsugamushi genotypes by intragenic recombination and their potential expansion in endemic areas. PLoS Neg Trop Dis 2017;11:e0005408. [CrossRef]
8. Xu G, Walker DH, Jupiter D, Melby PC, Arcari CM. A review of the global epidemiology of scrub typhus. PLoS Neg Trop Dis 2017;11:e0006062. [CrossRef]
9. Wu Y, Qian Q, Zhang W, Magalhaes R, Li S, Liu Y, et al. Rapid increase in scrub typhus incidence in mainland China, 2006-2014. Am J Trop Med Hyg 2016;94:532-6. [CrossRef]
10. Kinoshita H, Arima Y, Shigematsu M, Sunagawa T, Saijo M, Oishi K, et al. Descriptive epidemiology of rickettsial infections in Japan:Scrub typhus and Japanese spotted fever, 2007-2016. Int J Inf Dis 2021;105:560-6. [CrossRef]
11. Kweon S, Choi J, Lim H, Kim J, Kim K, Ryu S, et al. Rapid increase of scrub typhus, South Korea, 2001-2006. Emerg Inf Dis 2009;15:1127-9. [CrossRef]
12. Lee HW, Cho PY, Moon SU, Na BK, Kang YJ, Sohn Y, et al. Current situation of scrub typhus in South Korea from 2001-2013. Para Vect 2015;8:1-4. [CrossRef]
13. Lee Y, Wang P, Tseng S, Ko C, Teng H. Epidemiology of scrub typhus in Eastern Taiwan, 2000-2004. Jap J Inf Dis 2006;59:235.
14. Paris D, Walker D, Day N, Shelite T. Unresolved problems related to scrub typhus:A seriously neglected life-threatening disease. Am J Trop Med Hyg 2013;89:301-7. [CrossRef]
15. Chang K, Lee NY, Ko WC, Tsai JJ, Lin WR, Chen TC, et al. Identification of factors for physicians to facilitate early differential diagnosis of scrub typhus, murine typhus, and Q fever from dengue fever in Taiwan. J Micro Immu Inf 2017;50:104-11. [CrossRef]
16. Chakraborty S, Sarma N. Scrub typhus:An emerging threat. Ind J Derm 2017;62:478.
17. Mahajan S, Rolain J, Kashyap R, Bakshi D, Sharma V, Singh Prasher B, et al. Scrub typhus in himalayas. Emerg Inf Dis 2006;12:1590-2. [CrossRef]
18. Mathai E, Rolain J, Verghese G, Abraham O, Mathai D, Mathai M, et al. Outbreak of scrub typhus in Southern India during the cooler months. Ann N Y Aca Sci 2003;990:359-64. [CrossRef]
19. Patnaik S, Swain N, Sahoo B, Mishra R, Jain MK. Emergence of scrub typhus in Odisha-A hospital based study. Ann Trop Med Public Health 2017;10:636.
20. Mohanty L, Dhanawat A, Gupta P, Maheshwari G. Clinical manifestations and associated complications of scrub typhus in Odisha, India. J Clin Diag Res 2020;14:OC14-8. [CrossRef]
21. Sarangi R, Pradhan S, Debata N, Mahapatra S. Clinical profile of scrub typhus in children treated in a tertiary care hospital in eastern India. Ped Pols 2016;91:308-11. [CrossRef]
22. Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S. Outbreak of scrub typhus in Pondicherry. J Assoc Phys India 2010;58:24-8.
23. Dhar S, Kabi S, Das C, Samant S, Tripathy D, Kumar A, et al. Clinical spectrum of scrub typhus in a tertiary care hospital at Eastern India. Asian J Pharm Clin Res 2018;11:351. [CrossRef]
24. Mohakud N, Das P, Singh D, Das M, Nayak R. Epidemiological and clinical features of scrub typhus in Odisha, Eastern India. Med J Dr D Y Patil Vidyapeeth 2019;12:419. [CrossRef]
25. Takhar R, Bunkar M, Arya S, Mirdha N, Mohd A. Scrub typhus:A prospective, observational study during an outbreak in Rajasthan, India. Nat Med J India 2017;30:69.
26. Mahajan SK, Sharma S, Kaushik M, Raina R, Thakur P, Taneja GP, et al. Scrub typhus presenting as acute cerebellitis. J Assoc Phys India 2016;64:69-70.
27. Varghese G, Janardhanan J, Mahajan S, Tariang D, Trowbridge P, Prakash J, et al. Molecular epidemiology and genetic diversity of orientia tsutsugamushi from patients with scrub typhus in 3 regions of India. Emerg Inf Dis 2015;21:64-9. [CrossRef]
28. Dass R, Deka N, Duwarah S, Barman H, Hoque R, Mili D, et al. Characteristics of pediatric scrub typhus during an outbreak in the North Eastern region of India:Peculiarities in clinical presentation, laboratory findings, and complications. India J Pediatr 2011;78:1365-70. [CrossRef]
29. Vaz L, Gupta N. Outbreak of scrub typhus in Jammu-a report. Med J Armed Forces India 2006;62:342-3. [CrossRef]
30. Singh S, Devi K, Tilotama R, Ningombam S, Gopalkrishna Y, Singh T, et al. An outbreak of scrub typhus in Bishnupur district of Manipur, India, 2007. Trop Doc 2010;40:169-70. [CrossRef]
31. Krishna M, Vasuki B, Nagaraju K. Scrub typhus:Audit of an outbreak. India J Pediatr 2015;82:537-40. [CrossRef]
32. Gurung S, Pradhan J, Bhutia P. Outbreak of scrub typhus in the North-East Himalayan region-Sikkim:An emerging threat. India J Med Microc 2013;31:72. [CrossRef]
33. Viswanathan S, Muthu V, Iqbal N, Remalayam B, George T. Scrub typhus meningitis in South India-a retrospective study. PLoS One 2013;8:e66595. [CrossRef]
34. Subbalaxmi M, Madisetty M, Prasad A, Teja V, Swaroopa K, Chandra N, et al. Outbreak of scrub typhus in Andhra Pradesh--experience at a tertiary care hospital. J Assoc Phys India 2014;62:490-6.
35. Saifudheen K, Sajeeth Kumar K, Veena V, Gafoor V, Jose J. First case of scrub typhus with meningoencephalitis from Kerala:An emerging infectious threat. Ann India Acad Neur 2012;15:141. [CrossRef]
36. Sinha P, Gupta S, Dawra R, Rijhawan P. Recent outbreak of scrub typhus in North Western part of India. India J Med Micro 2014;32:247. [CrossRef]
37. Stephen S, Sangeetha B, Ambroise S, Sarangapani K, Gunasekaran D, Hanifah M, et al. Outbreak of scrub typhus in Puducherry &Tamil Nadu during cooler months. India J Med Res 2015;142:591. [CrossRef]
38. Sharma N, Biswal M, Kumar A, Zaman K, Jain S, Bhalla A. Scrub typhus in a tertiary care hospital in North India. Am J Trop Med Hyg 2016;95:447-51. [CrossRef]
39. Singh R. A study of etiological pattern in an epidemic of acute febrile illness during monsoon in a tertiary health care institute of Uttarakhand, India. J Clin Diag Res 2014;8:MC01. [CrossRef]
40. Usha K, Kumar E, Kalawat U, Kumar B, Chaudhury A, Gopal D. Molecular characterization of Orientia tsutsugamushi serotypes causing scrub typhus outbreak in southern region of Andhra Pradesh, India. India J Med Res 2016;144:597.
41. Mittal M, Thangaraj J, Rose W, Verghese V, Kumar C, Mittal M, et al. Scrub typhus as a cause of acute encephalitis syndrome, Gorakhpur, Uttar Pradesh, India. Emerg Inf Dis 2017;23:1414-6. [CrossRef]
42. Bora T, Khan S, Jampa L, Laskar B. Genetic diversity of Orientia tsutsugamushi strains circulating in Northeast India. Transactions of India. Roy Soc Trop Med Hyg 2018;112:22-30. [CrossRef]
43. Sahu S, Misra SR, Padhan P, Sahu S. Scrub typhus in a tertiary care hospital in the eastern part of Odisha. Apol Med 2015;12:2-6. [CrossRef]
44. Rao P, van Eijk A, Choubey S, Ali S, Dash A, Barla P, et al. Dengue, chikungunya, and scrub typhus are important etiologies of non-malarial febrile illness in Rourkela, Odisha, India. BMC Inf Dis 2019;19:572. [CrossRef]
45. Bal M, Mohanta M, Sahu S, Dwibedi B, Pati S, Ranjit M. Profile of pediatric scrub typhus in Odisha, India. India Pediatr 2019;56:304-6. [CrossRef]